

Extracted From:
http://sg.images.search.yahoo.com/search/images?p=agar+plates&fr=yfp-t-img&ei=utf-8&js=1&x=wrt
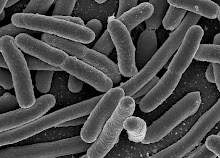
Bacterial requirements for growth include sources of energy,”organic" carbon (e.g. sugars and fatty acids) and metal ions (e.g. iron). Optimal temperature, pH and the need (or lacks of need for oxygen) are important.
A bacterial isolate can be classified into one of the five major groups :
• An aerobic organism that requires oxygen for cellular respiration, as well as free molecular oxygen in its surroundings for growth.
• Require an atmosphere that contains 20%-21% of oxygen.
• Examples: Mycobacterium tuberculosis (acid-fast) and Bacillus (Gram-positive).
Microaerophilic aerobe
• Microaerophilic bacteria grow well in low concentrations of oxygen, but are killed by higher concentrations.
• Require an atmosphere that contains less than 5% of oxygen.
• Example: Neisseria gonorrhoeae
Facultative anaerobe
• Facultative anaerobes can perform both fermentation and aerobic respiration. In the presence of oxygen, anaerobic respiration is generally shut down and these organisms respire aerobically.
• Capable of surviving in either presence or absence of oxygen.
• Example: family of Enterobactericeae, streptococci and staphylococci.
Aerotolerant anaerobes
• Aerotolerant anaerobes are bacteria that respire anaerobically, but can survive in the presence of oxygen.
• Grows better in the absence of oxygen but can survive in atmosphere containing air and a carbon dioxide incubator.
Obligate anaerobes
• Obligate anaerobes do not carry out oxidative phosphorylation. Furthermore, they are killed by oxygen; they lack certain enzymes which detoxify both H2O2and oxygen free radicals produced as side-products during metabolism in the presence of oxygen.
• Grow in the absence of oxygen.
Nutrient Requirements
These include sources of organic carbon, nitrogen, phosphorus, sulphur and metal ions including iron. Bacteria secrete small molecules that bind iron. Siderophores are then internalized via receptors by the bacterial cell. The human host also has iron transport proteins. Thus bacteria that ineffectively compete with the host for iron are poor pathogens.
Temperature Requirements
Bacteria may grow at a variety of temperatures from close to freezing to near to the boiling point of water. Those that grow best at the middle of this range are referred to as mesophiles; which includes all human pathogens and opportunists.
pH Requirements
Many bacteria grow best at neutral pH; however certain bacteria can survive and even grow in quite acid or alkaline conditions.
Biochemical and Metabolic Activities Test
Enzymatic activities
• Enzymes are biological catalysts, or chemicals that speed up the rate of reaction between substances without themselves being consumed in the reaction
• Enzymes can accelerate, often by several orders of magnitude, reactions that under the mild conditions of cellular concentrations, temperature, pH, and pressure would proceed imperceptibly in the absence of the enzyme.
• Widely used to differentiate bacteria.
Oxidase Test
• The oxidase test is a key test to differentiate between the families of Pseudomonadaceae (ox +) and Enterobacteriaceae (ox -)
• The enzyme cytochrome oxidase is involved with the reduction of oxygen at the end of the electron transport chain. The colourless reagent used in the test will detect the presence of the enzyme oxidase and, reacting with oxygen, turn a colour.
• Positive Reaction = Purple Colour

Picture Extracted From: http://www.mc.maricopa.edu/~johnson/labtools/Dbiochem/oxi.html
Ability to utilize carbon compound
• Ability to ferment/utilize selected carbohydrate
• An example could be the ability to use glucose or citric acid as carbon source
Characteristics of waste or breakdown products
• In any given environment, certain bacteria are characterized by their product of metabolic activities.
• Examples: Products of CO2, H2S, O2, acid or methane.
Differences in metabolic pathways
• Both autotrophs and heterotrophs must break down carbon compounds to release the energy they contain to sustain their own metabolism. This breakdown process is called respiration and it occurs at all times in all living cells of all organisms, plants, animals and bacteria. Fungi and bacteria break down the carbon compounds in dead animals and plants and convert the carbon to carbon dioxide if oxygen is present, or methane if oxygen not present.
Special Media
Selective Media
Selective media are used for the growth of only select microorganisms. For example, if a microorganism is resistant to a certain antibiotic, then that antibiotic can be added to the medium in order to prevent other cells, which do not possess the resistance, from growing.
Differential Media
Differential media or indicator media distinguish one microorganism type from another growing on the same media. This type of media uses the biochemical characteristics of a microorganism growing in the presence of specific nutrients or indicators added to the medium to visibly indicate the defining characteristics of a microorganism.
Mannitol Salt Agar
Mannitol Salt Agar (MSA):
• as a selective medium.
• A high concentration (7.5%-10%) of salt NaCl
• It is selective for members of the family Micrococcaceae and Staphylococcus since this level of NaCl is inhibitory to most other bacteria.
• as a differential medium.
• Acid production as a result of mannitol fermentation. Mannitol fermenters produce a yellow colony while non-mannitol fermenters will produce a reddish/purple colony.
• Sodium chloride is the inhibitory agent.
• Phenol red is the pH indicator.

 Staphylococcus aureus and Serratia marcescens
Staphylococcus aureus and Serratia marcescens
• S. epidermidis and S. aureus on selective/differential Mannitol Salt Agar
• The Staphylococcus aureus ferments mannitol and turns the medium yellow.
• The Serratia marcescens does not grow because of the high salt content.
Picture Extracted From: http://faculty.mc3.edu/jearl/ML/ml-8.htm
http://www.austincc.edu/microbugz/mannitol_salt_agar.html
MacConkey Agar
MacConkey Agar:
• as a selective medium.
• Distinguish lactose-fermenting Gram-negative organisms from non-fermenters.
• Crystal violet, bile salts and neutral red are inhibitory agents.
• Inhibit most Gram-positive bacteria, except Enterococcus and some species of Staphylococcus.
• as a differential medium.
• Neutral red is the pH indicator.
• Non-Lactose fermenting bacteria use peptone instead. This forms ammonia, which raises the pH of the agar, and leads to the formation of white/colourless colonies.
• Lactose fermenting bacteria produce acid, which lowers the pH of the agar below 6.8 and results in the appearance of red/pink colonies.
Klebsiella pneumoniae ferments lactose and - E. coli and Proteus on selective /differential produces pink colonies on MAC. Micrococcus luteus does not grow in the pre presence of bile salts and crystal violet.
Picture Extracted From: http://www.austincc.edu/microbugz/html/macconkey_agar.html
Nutrient Agar
It is a growth medium used to culture microorganisms. Selective growth compounds may also be added to the media, such as antibiotics.
• Contains 0.5% gelysate peptone, 0.3% beef extract, and 1.5% agar, and will support the growth of many organisms which are not nutritionally fastidious.
• Individual microorganisms placed on the plate will grow into individual colonies.

Control of a Nutient Agar: http://zoology.okstate.edu/zoo_lrc/biol1114/study_guides/labs/lab9.htm
Streak Isolation on Nutrient: http://faculty.mc3.edu/jearl/ML/ml-8.htm
Agar Colonies on Agar: http://www.usm.maine.edu/toxicology/research/uranium.php
Blood Agar
• Consists of a basal medium such as TSA enriched with 5% sheep blood or in some locations, horse blood. This is the most commonly used medium, and supports the growth of most of the common fastidious organisms, as well as, all of the less fastidious organisms.
• Blood agar is not selective as almost any type of microbe can grow on it.
• It identifies different bacteria based on their pattern of hemolysis.
Alpha hemolysis (α-hemolysis) is present if there is a greenish darkening of the agar under the colonies. Alpha hemolysis is generally caused by peroxides produced by the bacterium. Streptococcus pneumoniae and Streptococcus viridans display alpha hemolysis.
http://telem.openu.ac.il/courses/2007a/c20237/gifs/gallery/alpha_hemolysis.htm
http://www1.indstate.edu/thcme/micro/hemolys.html
Beta hemolysis (β-hemolysis) indicates a zone of clearing in the blood agar in the area surrounding a bacterial colony. It is caused by a complete lysis of the red cells in the media. The area around and under the colonies are lightened and transparent. Streptococcus pyogenes as well as some strains of Staphylococcus aureus display beta hemolysis.
http://www.as.ysu.edu/~crcooper/3702Laboratory(F04).html
http://www1.indstate.edu/thcme/micro/hemolys.html
Gamma-hemolysis is actually a lack of hemolysis in the area surrounding a bacterial colony growing on blood agar. In fact, culture of bacteria on blood agar for the purpose of hemolysis classification is performed at 37oC in the presence of 5% CO2. This results in an overall brownish discoloration of the blood agar, from its original blood-red hue.
http://sg.images.search.yahoo.com/search/images?p=Gamma+hemolysis+&fr=yfp-t-img&ei=utf-
http://www.jlindquist.net/generalmicro/dfhemo.html
Serology Testing
• It is the scientific study of blood serum.
• Usually refers to the diagnostic identification of antibodies in the serum.
• May be performed for diagnostic purposes when an infection is suspected, in rheumatic illnesses, and in many other situations, such as checking an individual's blood type.
• Help to diagnose patients with certain immune deficiencies associated with the lack of antibodies.
• There are several serology techniques that can be used depending on the antibodies being studied. These include agglutination, precipitation, complement-fixation and fluorescent antibodies. • Some serological tests are not limited to blood serum, but can also be performed on other bodily fluids such as semen and saliva, which have similar properties to serum.
Slide Agglutination Test
• A rapid screening or semi quantitative test in which antibody and antigen are mixed on a glass slide and observed for agglutination.
• Antigen-antibody combine to form clumps which can be visualized by naked eye.
• Cannot be performed if the bacterial suspension is granular, auto agglutinates or is sticky.
• Unknown bacterial isolates are mixed with antisera to know bacteria.
• In some cases, serum from patients is mixed with known bacterial antigens to identify the antibodies in them and thus the source of infection.
• Positive slide agglutination indicates immune mediated hemolytic anemia.
• A negative result does not rule out immune disease.
Enzyme-Linked ImmunoSorbent Assay
(ELISA)
• Enzyme-Linked ImmunoSorbent Assay: is a biochemical technique used mainly in immunology to detect the presence of an antibody or an antigen in a sample.
• Used as a diagnostic tool in medicine and plant pathology, as well as a quality control checks in various industries.
• It is a useful tool both for determining serum antibody concentrations and also for detecting the presence of antigen.
• ELISA can also be used in toxicology as a rapid presumptive screen for certain classes of drugs.
http://www.biotech-weblog.com/50226711/enzymelinked_immunosorbent_assay_elisa_35_years_after.php

No comments:
Post a Comment